Keith Fontenot, Caitlin Brandt and Mark B. McClellan
February 2, 2015 9:59am - Brookings Institution
A Primer on Medicare Physician Payment Reform and the SGR
If there is an equivalent of gGroundhog Dayh in the
legislative arena, it may be the semi-annual exercise to defer the physician
payment rate cuts called for in Medicarefs Sustainable Growth Rate (SGR)
legislation. Ever since 2003, Congress has legislated an alternative to the
automatic cuts scheduled under the law. This time, absent legislative action,
payments to physicians under Medicare will but cut by 21.2 percent starting in
April.
Last year, the three Congressional committees with
jurisdiction over Medicare came together on a bipartisan, bicameral plan to fix
the flawed system permanently. The remainder of this post explains just
what is behind this decade of gkicking the can down the road.h
For more details on how the Medicare SGR bill can be
enhanced through alternative payment models, we recommend reading,
"Medicare
Physician Payment Reform: Securing the Connection Between Value and
Payment" and Alice Rivlin's prepared
testimony to the House Committee on Energy and Commerce
Subcommittee on Health from January 21.
What is the Medicare Sustainable Growth Rate?
Put in place through the Balanced Budget Act of 1997, the SGR is a system
designed to control the costs of Medicare payments for physicians. The SGR
formula was aimed at limiting the annual increase in cost per Medicare
beneficiary to the growth in the national economy. The SGR is layered on top of
a system for paying physicians known as a gphysician fee schedule,h which pays
physicians for delivering a number of individual Medicare services ("volume"),
rather than for quality or keeping people healthy ("value").
Under the SGR formula, if overall physician costs exceed target expenditures,
this triggers an across-the-board reduction in payments. The target is
based on spending growth in the economy – thatfs where the gsustainableh part of
the name comes from – but is not tied to quality or access to care. This year,
if Congress does not act by March 31, then payments to Medicare physicians would
be reduced by 21.2 percent. However, since 2002, Congress has stepped in with
short-term legislation (often referred to as the gdoc fixh) to avert the payment
reduction. These patches have kept increases in physician payments below
inflation over time, and have also resulted in a huge divergence between the
actual level of Medicare physician-related spending and the target in the SGR
formula. Consequently, the budgetary cost of permanently fixing the SGR now runs
over a hundred billion dollars. For years it has been clear that both the SGR
and physician payment system urgently need attention.
Why is the SGR such a significant problem?
Several important consequences of this outdated and
inefficient process are described below. Overall, the SGR:
Disregards individual and group performance. Because
the SGR is merely a system of budget controls it does nothing to give an
individuals or physician groups any incentives for performing more efficiently.
Regardless of how poorly or how well physicians may do on quality or efficiency
of care they are nonetheless subject to the aggregate cut.
Makes physician payments uncertain every
year. The instability caused by the threat of payment cuts is detrimental to
Medicare physicians and the program. While the formula has been
bypassed, it is difficult for clinicians to plan for the future, let
alone have the certainty they need to reform and improve care.
Distracts from other legislative priorities. Preparing
annual legislation to avoid falling off the SGR cliff chews up valuable
Congressional time. Congress has so little time and so much else to do that an
annual SGR patch diverts attention from other important issues including
implementing better payment models.
Defers program improvements. The high cost of permanent
repeal – in the range of $150 billion over ten years -- has effectively locked
us in to a pattern of annual extensions that has thus far stymied Congressional
reform efforts.
Presents a threat to health of seniors. Although surveys
have not shown significant deterioration in beneficiary access at the national
level, the standard for payment in Medicare should not be whether or not
problems of access to care have reached a substantial level.
How did we get in this mess?
It is important to remember that the SGR was an attempt by
Congress to address a very real problem: the underlying physician payment
system pays physicians for providing more, not better care.
Previous efforts at controlling the cost of physician spending in Medicare
had proven ineffective and so in 1997 Congress adopted the SGR formula.
Recall that the formula ties physician payments to growth in
the national economy. In the late 90s, while economic growth was high and
medical cost growth was low, the system produced increases in physician payments
and no cuts were necessary. In 2001, however, the combination of a
recession (declining GDP) and increasing medical costs led to an automatic cut
of 4.8 percent in 2002, and each year thereafter.
This also exacerbated the problem because of the
cumulative nature of the SGR. To minimize the budgetary impact of the gdoc fixh,
Congress actually increased the reduction in succeeding years to make up
for the cost of the fix in the current year. For example, if the formula called
for two years of five percent cuts, Congress instead legislated one year of no
cut and one year of a ten percent cut. This approach has led to the looming 21.2
percent cut.
Why does SGR cost so much?
Under current law, physician payments are scheduled to be
reduced. Measured against that gbaselineh of spending, the legislative action to
maintain current payments does score as a cost. However, Congress also
operates under a requirement to pay for the costs of new legislation so most SGR
extensions have included adjustments to other health related payments, such as
an extension of the Medicare sequester. So in that sense, the SGR has functioned
to create pressure to hold down costs, just not in the way the SGR formula
intended.
Moreover, the need to offset spending has led to a squeeze on
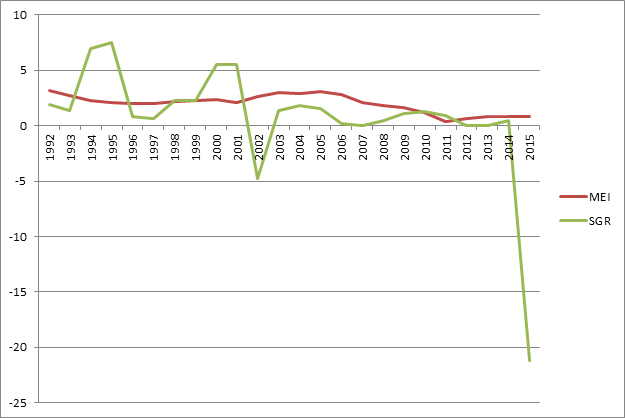
physician payment rates over the past dozen or so years. Figure 1 below
compares the Medicare Economic Index (MEI), a measure of physician practice cost
inflation, to the actual SGR updates from 1992 through the scheduled 2015
changes. At points in the past the annual updates for physician payments
greatly exceeded the MEI, but since about 2001, they have generally been below
the MEI. So while the formula has not operated as it was designed since 2002 it
has placed significant limits on increases in reimbursement for physician
services.
Figure 1. Medicare Economic
Index and Sustainable Growth Rate Comparison
How can we permanently fix this flawed system?
The most important thing we can do to continue to push health
reform forward is to move away from our current gfee for serviceh system.
Instead, we must transition to payment models that involve greater
accountability for providers for the quality and cost of the care they deliver.
A more effective payment system would recognize that physician decisions have
significant impacts on overall health care costs, and better
support physicians to make improvements in the delivery of care. In
addition, many services that physicians provide – from responding to emails, to
helping patients develop care plans– are not supported by the current
fee-for-service payment system. Last year's tri-committee bill
was developed around a proposal to replace the SGR with a new system that
supported galternative payment modelsh, such as Accountable Care Organizations
(ACOs), bundled payments and patient-centered medical homes. Though it
could be improved, this legislation is a good start. For more information on the
implementation of alternative payment models, read our Medicare
reform health policy brief.
What is the potential for actually getting something done?
This is a huge challenge. The cost of last yearfs legislation
is in the range of $150 billion over ten years. And unfortunately there
has been virtually no discussion of how to pay for it. Elsewhere, we wrote
about how
to pay for a permanent SGR fix, and suggested that if such a discussion
proves to be too challenging, then Congress should consider a semi-permanent fix
in the three to five year range. It is critical that physicians have a
period of stability and incentives to invest in the management tools that will
help them move away from the current, inefficient, fee for service models.
With a new Congress it remains to be seen how this will
proceed. There are new Chairmen in two of the major committees – House Ways
and Means and Senate Finance. While they support reforming the SGR system it is
possible that they will want to review last yearfs legislation and consider
changes. With the current gpatchh expiring in March, some action will have
to be taken quickly to avoid precipitous payment cuts. Because there
is little time before then to develop consensus around the legislation and how
to pay for it, the odds again favor some sort of further short term extension.
But this could be done in a way that facilitates a permanent or semi-permanent
fix soon, perhaps in this Congress. If Congress, adopts a new budget and moves
to implement it, it is quite possible SGR will be included as one of those
items. That process, however, can take several months to unfold.
Keith Fontenot
Visiting Scholar, Economic
Studies, Engelberg
Center for Health Care Reform
Keith Fontenot is a visiting scholar in the
Engelberg Center for Health Reform, under the Economic Studies program at the
Brookings Institution. Mr. Fontenot is veteran of budget, legislative and
analytical issues surrounding the nation's health and other major entitlement
programs.
Caitlin Brandt
Research Analyst, Economic
Studies, Engelberg
Center for Health Care Reform
Mark B. McClellan
Director, Health Care Innovation and Value Initiative
Senior Fellow, Economic
Studies
Mark McClellan, MD, PhD, is a senior fellow and director of the Health Care
Innovation and Value Initiative at the Brookings Institution. Within
Brookings, his work focuses on promoting quality and value in patient centered
health care. A doctor and economist by training, he also has a highly
distinguished record in public service and in academic research. Dr. McClellan
is a former administrator of the Centers for Medicare & Medicaid Services
(CMS) and former commissioner of the U.S. Food and Drug Administration (FDA),
where he developed and implemented major reforms in health policy. These
include the Medicare prescription drug benefit, the FDAfs Critical Path
Initiative, and public-private initiatives to develop better information on
the quality and cost of care. Dr. McClellan chairs the FDAfs Reagan-Udall
Foundation, is co-chair of the Quality Alliance Steering Committee, sits on
the National Quality Forumfs Board of Directors, is a member of the Institute
of Medicine, and is a research associate at the National Bureau of Economic
Research. He previously served as a member of the Presidentfs Council of
Economic Advisers and senior director for health care policy at the White
House, and was an associate professor of economics and medicine at Stanford
University.